A motivational message for the day

Oooops! – Owl
Tom Whipple, Science Editor | Kat Lay, Health Editor www.thetimes.co.uk
Government modelling from two weeks ago underestimated the level of hospital admissions by more than a third, according to newly released documents.
Projections produced by Spi-M, the Sage modelling committee, on June 28 estimated that there would probably be about 275 daily hospital cases in England by about July 6, with an upper estimate of 350.
In reality on July 7, the latest date for which figures are available, there were 461 people admitted to hospital in England, and admissions were rising at a significantly higher rate than expected.
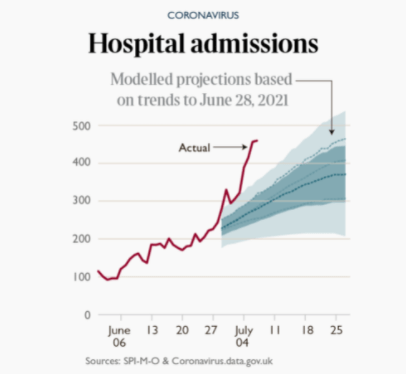
The discrepancy suggests that crucial decision-making at the time around reopening would have been informed by assumptions that turned out to be overly optimistic.
However, it came after a period when admissions had been significantly below those predicted by earlier models,which led some Sage scientists at the time to suggest that the delay to reopening might have been unnecessary.
Dr Stephen Griffin, from the University of Leeds, said that continued confusion over hospital admissions and their link to cases highlighted the uncertainty in relaxing restrictions.
“While we can’t say for sure that hospitalisations might follow this precise trajectory, it seems likely that they will track the exponential growth in cases we are seeing. Thus, as many are predicting, the dropping of restrictions on July 19 represents an unacceptable and unnecessary risk,” he said.
Neither should hospital cases be viewed as the only relevant metric. “There seems no accounting whatsoever of morbidity in the government plans, and there will be many, including younger people and children, that become seriously unwell,” he said. “Even before the 19th, Delta is out of control, we must not let this run rampant, let alone add more fuel to the fire.”
One of the key concerns about high caseloads over the winter appeared to have been tempered yesterday, with data from Public Health England [PHE] showing that two vaccine doses offered strong protection for most of those who are immunosuppressed.
The study involved a million participants with different conditions that made them clinically vulnerable. It found that overall in this group both the Oxford-AstraZeneca and Pfizer- BioNTech jabs offered 60 per cent protection after one dose. After two doses, the AstraZeneca vaccine offered 80 per cent protection from symptomatic disease. The Pfizer jab offered 89 per cent protection for over-65s, but data was unavailable for younger people.
Among those whose immune systems had been compromised, there was only 4 per cent protection after a first dose, but 73 per cent after a second.
The figures come with some uncertainty due to the smaller numbers involved. Blood Cancer UK said it was also concerned that people with different immune problems were grouped together. Gemma Peters, chief executive of Blood Cancer UK, said: “While there is a lot of uncertainty, there is enough reason to think the vaccines may not work as well for some people with blood cancer to continue to be cautious even after having both doses.”
Dr Mary Ramsay, head of immunisation at PHE, said the findings showed it was vital that anyone with an underlying condition got both doses.
First an extract from this week’s letter to the “Lancet” criticising Boris Johnson’s “If not now, when?” freedom day strategy.
“Fourth, this strategy will have a significant impact on health services and exhausted health-care staff who have not yet recovered from previous infection waves. The link between cases and hospital admissions has not been broken, and rising case numbers will inevitably lead to increased hospital admissions, applying further pressure at a time when millions of people are waiting for medical procedures and routine care.”
Second in May 2020 Owl wrote:
Owl hears a lot about NHS capacity being measured in terms of the supply of PPE, number of beds and ventilators etc, not much about the limits of human endurance. In a couple of articles Owl has posted recently, Max Hastings has drawn comparisons between this emergency and the way resources are, or have been, mobilised in war. One wartime experience is a recognition of “battle fatigue” and the need to manage this through “troop rotation” (either as individuals or as units) to maintain full efficiency. (Owl uses the recognised military terms tofacilitate research searches.)
Frontline NHS staff have been working at full stretch in extremely stressful conditions. It is unlikely that this peak work rate could, or should, be sustained indefinitely.
Today, we have:
‘Dread and anxiety’ among NHS staff as Covid cases surge again
Denis Campbell www.theguardian.com
“NHS staff have a sense of dread about what’s around the corner. While we understand things need to open up some time, the timing feels like utter madness while we are so close to successfully vaccinating the population, and with a more contagious variant circulating.”
That view, expressed by a frontline respiratory consultant, is widely shared across the NHS. The doctor concerned has already grappled with the first two waves of Covid. She is now steeling herself for the next one which, despite being in its early stages, has already led one major hospital trust, in Leeds, to cancel scheduled surgery, including several cancer operations.
Among an NHS workforce weary after 16 months dealing with the pandemic there is a mixture of apprehension, nervousness, fear, a here-we-go-again resignation at the return of a familiar foe, stoical readiness to do their best again, and also anger that they will have to.
The same doctor adds: “We’ve seen a steady increase in [Covid] numbers over the past few weeks and are back to having a full Covid ward and patients on intensive care. While they are overall a lot younger, sadly deaths are slowly creeping up despite this.
“Healthcare professionals are deeply anxious about the impact of relaxing restrictions further given the current surge in Covid cases. To do away with risk-mitigating measures like social distancing and wearing of masks is incomprehensible to many of us. I feel anxious and frustrated.
“The dread and anxiety are because we’ve been here before, we’ve lived through the first two – or three depending on where you are – waves. We don’t want to be back in that place where we are on ‘escalation’ rotas, routine work is cancelled and we are dealing with deaths that we believe could have been preventable with a better public health strategy.”
Dr Nick Scriven, the immediate past president of the Society for Acute Medicine, who works in a hospital in Yorkshire, says: “Us up north are experiencing a fourth wave in community cases, with an uptick in hospital cases. Although numbers are not massive it’s both frightening and upsetting for staff as ICU cases are rising with unvaccinated people, either as they are young or by choice or both. There is to me a growing feeling that vaccination makes this almost preventable.”
However, doctors and hospital bosses are a bit more relaxed about the coming next surge in cases because they expect it to be different to the intensely demanding first two: smaller, less dramatic and less likely to cripple the NHS. Dr Rupert Pearse, an intensive care consultant in London, tweeted sardonically last weekend to say: “As we did in November 2020 we are projecting a ‘slow burn’ of hospital admissions rather than a third wave. Let’s hope our forecast is more accurate this time.”
Covid admissions to hospitals generally and intensive care units specifically are going up again, reflecting the sharp recent growth in infections. But the numbers involved remain low compared with spring last year and last winter, and the trajectory, while unmistakably upward, is nothing like as vertical as it was then.
Chris Hopson, the chief executive of hospital group NHS Providers, says: “For this set of variants, vaccines have broken the link between infections and previously high hospitalisations/mortality rates. So there’s high confidence among trust leaders that increasing community infection rates, even to the levels we saw in January, will not translate into the levels of hospitalisation and mortality we saw in that peak; a peak that brought extreme pressure to the NHS.”
But Hopson said in a thread of tweets this week on the NHS’s readiness to withstand the next wave that even a smaller surge in Covid cases posed a threat to a health service that is already – and official figures bear this out – the busiest it has ever been.
He pointed to the NHS’s efforts to tackle the huge backlog of people needing hospital treatment and deal with the record number of people turning up at A&E, while trying to give tired, stressed staff some much-needed time off and function with fewer beds than pre-pandemic because social distancing in hospitals means an eight-bed ward now contains just six. He is also increasingly concerned about the burden that the rising number of cases of “long Covid” is now placing on hospitals – a much less prevalent problem during the first and second waves.
Scriven says: “It’s overwhelming busy even without another Covid wave. Moving forwards, the government-projected rise [in infections to 100,000 a day] due to unlocking is a concern. Even if the hospital numbers don’t reach the same levels, the NHS is in a really difficult place. Any rise in Covid will seriously challenge elective [surgery] recovery and urgent and emergency care that is already struggling under the demand.”
Hopson and his counterpart at the NHS Confederation, Matthew Taylor, have warned in recent days that a new influx Covid-positive patients arriving when an overloaded, under-staffed service is facing winter-like demand for care in July would inevitably force hospitals to limit the amount of surgery they can perform. “Any significant Covid surge this summer will place even more strain on a system struggling to cope,” said Taylor.
With ministers putting pressure on the NHS to give the 5.3 million people on the waiting list in England the treatment they need as soon as possible, the service’s inability to do so – and the prospect of a fresh suspension of normal care – could become a key political issue.
Hopson points out that this time around the risk for the NHS is not “the likely absolute level of Covid-19 hospital admissions”, which thanks to the vaccination programme should be much lower than before. It is more about the next wave’s timing and the service’s underlying fragility after a decade of austerity funding and chronic staff shortages.
Delays to surgery can have consequences, he says ominously, suggesting they may prove unavoidable, depending on events outwith the health service’s control, especially what happens in England after “freedom day” on 19 July. “Trust leaders obviously have a mission to avoid any unnecessary harm. So they are instinctively uneasy about potential harm to any patient. But they also recognise wider issues at stake here.”
Some of you may have noticed a group of planning applications validated for week beginning 21 June for a number of car parks on the Pebblebed Heaths.
They are grouped under this group application. and cover Stowford Woods, Frying Pan, Four Firs and Joneys Cross.
It is a response to the increased “footfall” pressures caused by “build, build, build”. Note the phrases “gathering” and “flexible visitor management” – Owl
Extracts from Pebblebed Heaths Car park strategy 2019
The primary objective of this car parking strategy is to safeguard the SPA protected bird species (Nightjar and Dartford Warbler) and SAC heathland habitats from the adverse impacts and disturbance caused by people, particularly from dogs that are not on a lead. The principles applied to the car parking strategy seek to achieve this through: –
…..Whilst this report does not recommend charging for parking to manage visitor numbers, as payment for parking at formal car parks is likely to displace visitors across the SPA/SAC undoing the principle of gathering visitors at nodes, the report does discuss charging options being adopted by other countryside managers.