“… In Norfolk and Waveney, the latest Sustainability and Transformation Plan (STP), under guidance from NHS England, has only been seen by a small group of health chiefs.
It has been kept from MPs, councillors, NHS staff, GPs, unions and some hospital board members.
An initial version of the plan was published in June, which warned there would be a deficit of £440m by 2020 in the NHS and social care budget, if action was not taken.
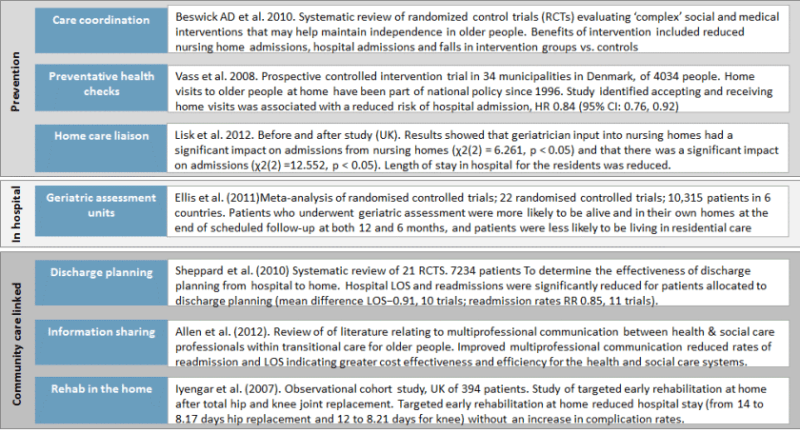
The plan proposed keeping patients out of hospital by expanding community and social care, but little detail has been given so far about what that action might be or how they hope to save a proposed £160m.
The full STP plans have been published in several areas of the country, but Norfolk and Waveney STP is following NHS England guidance by not making their proposal public yet.
Managing director of Norfolk County Council Dr Wendy Thomson, who is leading on the STP, said their plan was “at an earlier stage in its development compared to many others around the country.”
““Plans are not yet at the point where they have clear messages about things the public want to know”
Dr Wendy Thomson, Norfolk County Council
“Plans are not yet at the point where they have clear messages about things the public want to know,” she said.
“As service plans are developed, EDP readers can be assured that changes will be subject to the right public engagement and statutory consultation.” The Norfolk and Waveney STP is expected to be published in late November, but it is understood there will still be little detail in the document about what health chiefs propose to do with Norfolk an Waveney’s health system to plug the financial blackhole.
North Norfolk MP and former health minister Norman Lamb said there would be little hope of the getting the public involved in the plans if they were presented as a “fait accompli”.
He said he supported the idea of saving money by having more people being cared for in the community and joining up health and social care, but said the idea that hundreds of millions of pounds could be saved through STPs was fanciful.
“It is in the realms of fantasy to imagine this is achievable,” he said. “I don’t think when it is published people will get that excited about it. It will not say anything significant in terms of detail of changes. What lies beyond that is much more disturbing for many.”
Jeff Keighley, Unison regional organiser, said STP leaders should have consulted the public “at the earliest possible opportunity”.
Although the union said it was not against “sustainable transformation”, Mr Keighley said he was concerned the proposals would not be sustainable.
“If they had found a wonderful way of saving this money by enhancing the services it would be amazing – and they would have not been keeping it a secret,” Mr Keighley said. …
… What’s happening in other areas
Some councils have objected so strongly to the lack of public involvement they have ignored NHS England’s demand to keep the documents private until a later stage and have published them on their websites.
The plans on how local NHS areas will move forward over the next five years focus on several key themes.
These include cutting costs, moving care closer to home, putting a greater emphasis on preventing people becoming ill in the first place and concentrating services in a smaller number of units or hospitals.
Some argue this will enable increased access to consultants around the clock and make the best use of specialist NHS staff and resources. There are also plans to streamline back-office functions.
So far, more than a dozen plans have been published or leaked. Here are details from some of the key ones:
•The plan for Durham, Darlington, Tees, Hambleton, Richmondshire and Whitby set out how either Darlington or North Tees could lose their emergency department, with one becoming a “specialist emergency hospital” and another becoming a “local hospital”.
The plan says this will drive up standards, ensure a seven-day consultant presence with at least 16 hours per day consultant specialist access. More than 75% of patients could be assessed by a specialist consultant on admission and 100% assessed within 12 hours by a consultant.
Consolidating these services, together with other departments, could save millions of pounds, the plan said.
•The south-west London document outlines plans to cut the number of acute hospitals on the patch from five to four. Currently there are five hospitals at Croydon, Epsom, St Helier, St George’s and Kingston.
The plan says: “The only site which we believe is a ‘fixed point’ is St George’s Hospital in Tooting since it provides hyperacute stroke, major trauma and other services which are serviced by highly-specialised equipment and estates, which would be very expensive to re-provide elsewhere in south-west London.”
The document says reduction in sites is necessary to provide seven-day services with enough doctors and consultants – one of Health Secretary Jeremy Hunt’s main aims.
“We are very unlikely to be able to deliver services that meet clinical quality standards across five acute hospital sites. In particular, clinicians do not believe that we will be able to recruit or pay for sufficient workforce to deliver seven-day services at five acute sites.”
•In Birmingham and Solihull, the plan states that by 2021 there could be a deficit of £712 million across the health and care sector if nothing is done to address issues in the local health economy.
It says it will establish a single “lead provider” for maternity care and look to “immediately” implement a shared service for back-office functions across its four main acute providers and create a centralised laboratory for routine pathology work.
There are currently two main providers of maternity care – Birmingham Women’s Foundation Trust and at the Heart of England.
Plans to merge Birmingham Women’s and Birmingham Children’s Hospitals by next year have already been announced while University Hospitals of Birmingham and Heart of England FT announced in September the intention to create a “single organisation”.
•North-west London’s draft STP, seen by the Health Service Journal (HSJ) last month, aims to “consolidate acute services on to five sites” from the current nine.
Two London councils – Ealing and Hammersmith and Fulham – have said they cannot agree to a plan that assumes Charing Cross Hospital will be downgraded.
Stephen Cowan, leader of Hammersmith and Fulham council, said: “At the heart of the STP is an acceptance that Charing Cross Hospital will be demolished and replaced with significantly downgraded facilities, with the capital receipts from the sale of much of the hospital’s land intrinsic to the delivery of the STP. 1/8We are 3/8 strongly opposed to this, and therefore the STP.”
•The Cheshire and Mersey plan includes the downgrade of at least one A&E department along with a major consolidation of elective care.
The A&E at Macclesfield hospital would become a minor injuries unit. According to the Health Service Journal (HSJ), there will be a formal “major service review” at Southport and Ormskirk Hospital Trust, and the document includes options that could reduce the number of 24-hour A&E departments across three acute trusts.
•The north central London document sees officials over the next year examining whether some key services “would benefit from consolidation or networking”.
These services include maternity, out-of-hours emergency surgery, orthopaedics, mental health crisis care and dermatology.
http://www.edp24.co.uk/news/health/bid_to_transform_nhs_in_norfolk_and_waveney_and_save_160m_in_realms_of_fantasy_1_4774673