NHS staff shun testing centres amid concerns about safety and lost results
Contracts to operate testing facilities have been awarded under special pandemic rules, through a fast-track process without open competition. These include the accountants Deloitte, the public services specialists Serco and Sodexo, and the pharmacy chain Boots, which has also trained and provided more than 300 staff to administer swabs.
Owl wants to point out that if you decide, for expediency or ideology, to go down the contracting route for a complex sequence of operations then best practice would be to appoint an experienced prime contractor, with overall responsibility. Doesn’t seem to happened in this case.
“At Wembley tests have been lost, with no contact number provided to chase missing results. The site is operated by Sodexo, but the responsibility for ensuring staff get the results lies with Deloitte. The accounting firm is managing logistics and data across most of the test centres, including booking tests, getting samples to the labs and communicating the results.”
As a Royal Free source says: “…The chain of command is very opaque and it is very difficult to know how you get your results back. It should be run by people with operational experience of clinical tasks, not by an accountancy firm.”
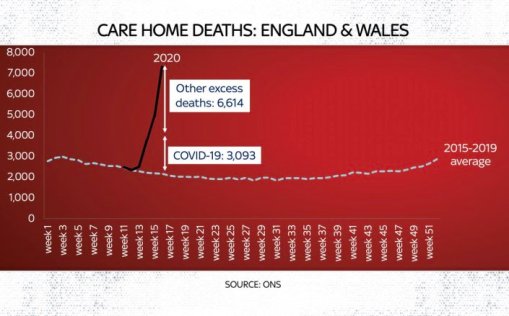
The other ideology that concerns Owl is the element of competition that has been allowed to creep into the allocation of the scarce resource of testing. Everyday the Government announces yet another group eligible for testing (possibly driven by the need to be seen to be ramping up testing). The result is that we are witnessing an unseemly scramble for who can get to the telephone, or on-line, first. Owl believes that whilst testing is still limited there has to a prioritised system of rationing, for example, currently to care homes and their staffs. No doubt this is anathema to those adhering to the right wing “the devil take the hindmost” principle.
For the article read on:
Juliette Garside, Lisa O’Carroll the Guardian 29 April 2020
Key workers and NHS staff have raised concerns about the management of a national network of drive-in corona-virus testing centres, with doctors at one London hospital trust “actively discouraging” staff from using them.
Thousands of people have turned up at more than 30 locations around the UK to be swabbed for traces of the virus after the government opened up facilities previously reserved for NHS workers to all employees in essential services, including care homes and utilities companies.
The expansion in testing at the weekend has led to long queues at some facilities, with motorists – many of them already feeling unwell with symptoms of Covid-19 – stuck in their cars in hot weather for hours, forbidden from opening windows and unable to use toilets or find water.
The Guardian was contacted about multiple concerns, including queues of up to five hours, workers with appointments turned away because of delays, leaking test vials, wrongly labelled samples, and lost test results at Nottingham and Wembley.
A doctor at the Royal Free NHS trust, which operates three hospitals in north London, said they were so concerned about the drive-in facility located in the Ikea car park in Wembley that staff had been told not to use it.
The regional network, which will be extended to 50 locations, is a cornerstone of the government’s target of reaching 100,000 coronavirus tests a day by the end of April.
Contracts to operate the facilities have been awarded under special pandemic rules, through a fast-track process without open competition.
The contracts were handed to private companies including the accountants Deloitte, the public services specialists Serco and Sodexo, and the pharmacy chain Boots, which has also trained and provided more than 300 staff to administer swabs.
At Wembley tests have been lost, with no contact number provided to chase missing results. The site is operated by Sodexo, but the responsibility for ensuring staff get the results lies with Deloitte. The accounting firm is managing logistics and data across most of the test centres, including booking tests, getting samples to the labs and communicating the results.
The Royal Free source said: “All three [of the trust’s] hospitals are actively discouraging people from going there. We have no faith that they would get the result. The chain of command is very opaque and it is very difficult to know how you get your results back. It should be run by people with operational experience of clinical tasks, not by an accountancy firm.”
Instead of using Wembley the trust is swabbing staff at work and sending samples to Francis Crick Institute laboratories for analysis.
People attending a number of drive-in facilities reported being left with no choice but to take their own swabs, having expected the procedure to be carried out by a trained professional.
James Collins, a carer at a home for vulnerable adults in Lincoln, who has been self-isolating with a cough, said he waited five hours fora test at Robin Hood airport, Doncaster, on Saturday; it had involved a two-hour round trip.
He was surprised to have to swab himself. “I’m scared I haven’t done the test right,” he said after testing negative. “If I wanted to do it myself I would have gone for a home test.”
At Doncaster and elsewhere security guards patrolled the lanes warning motorists not to take photos or videos and not to open their windows. Drivers could communicate with marshals only by phone. There were some portable toilets, but after a single use they were sealed, awaiting cleaning.
Serco, which runs nine centres including Doncaster, said the longestrecorded wait was two hours, adding: “Serco is managing the site facilities at some of the Covid-19 test facilities. The sites are becoming increasingly busy and we are working hard to get people through the centres as quickly as possible?’
Anna Wittekind, a nutritionist who said she had been off work with chest and stomach pains for 12 days, said she and her husband, who worked for the NHS, had waited three hours at a drive-in facility. Her result arrived quickly and was negative.
“I have no idea whether I managed to take a good enough swab, so it may have all been a waste of time,” she said. “I felt for the poor souls working there, but the organisation was abysmal.”
A worker at the Lighthouse laboratory in Milton Keynes said she was concerned about safety and lost results. The lab was opened by the health secretary, Matt Hancock, this month as one of three “megalabs” created to support the testing initiative.
She claimed the lab, which is capable of processing up to 10,000 tests in 24 hours, had received hundreds of swabs in vials that either were leaking or were not sealed in two bags, meaning those handling them risked contamination. Other swabs had labelling errors, so the results were unlikely to reach the person tested.
“We do feed these problems back to the test sites and some improve,” she said, “but some are consistently poor and in some cases this goes beyond just making our lives difficult to actively endangering us or the reliability of results?’
Steve Fay, a physiotherapist in respiratory care in Leicester, said he was seen at a centre in Nottingham operated by Boots on 1 April. He was left waiting for more than a week for the results. His wife, who works as an NHS nurse and had her test at the same time, had to wait even longer.
After chasing, via 14 emails, Fay was eventually referred to Deloitte.
Fay said: “I threatened to make this public when suddenly [there was] a reply in one hour and a result an hour later. The tests both came back negative. Personally I’m very doubtful of this test because we both had the symptoms?’
A spokesman for Deloitte said: “Deloitte has a specialist health sector practice, which includes a large number of staff with operational healthcare experience. This is the group who is at the core of our work, supplemented where appropriate with individuals with technical skills relevant to the work we are doing?’
Boots said it managed the Nottingham site but had “no role in processing the results”. Sodexo also said it was not responsible for delivering test results.
The Department of Health and Social Care said the latest records showed that more than 90% of people tested up to 21 April had received their results within two days.